Cdi Programs Are Best Applied in Which Situations
The participation of CDI in the CACFP creates unique situations requiring coordination and understanding between two Federal programs operated by one nationwide grantee. There is a shortage of qualified CDI specialists and ongoing budget limitations limit program expansion into outpatient and other settings.
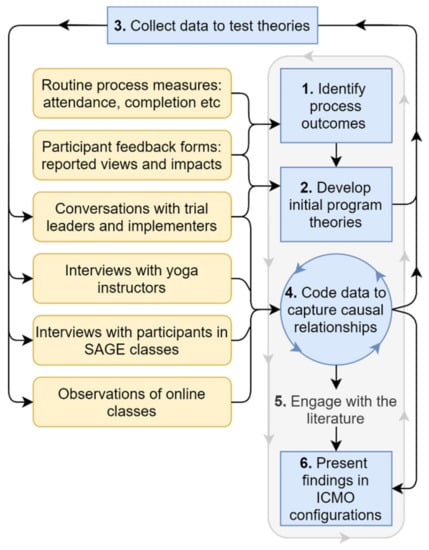
Ijerph Free Full Text Using Realist Evaluation To Understand Process Outcomes In A Covid 19 Impacted Yoga Intervention Trial A Worked Example Html
CDI provides programs on Organizational Consulting Facilitating Strategic Planning and Facilitating Board Development.

. Coded data is then translated into quality reporting physician report cards reimbursement public health data and disease tracking and trending AHIMA 2019. For example if the physician must consider co-morbidities when deciding a course of treatment the existence and status of those co-morbidities should be noted in the. The strategies are intended to facilitate implementation of CDI prevention efforts by state and local health departments quality improvement.
Most CDI programs begin in a hospital setting but programs are not limited to this setting. Making yourself more knowledgeable puts you in a more informed position when faced with documentation and coding challenges. Documentation deficiencies occur in both outpatient and inpatient settings but clinical documentation integrity CDI programs have been implemented primarily in the inpatient setting only.
Expand CDI audit scope. As the industry continues to move forward in value-based reimbursement we are seeing outpatient CDI efforts pop up in primary care specialty practices ambulatory surgery and emergency departments. CDI programs began with a focus on reimbursement but quickly shifted to concentrate on quality outcomes.
Whats the best approach. Cyber-Enabled Discovery and Innovation CDI Synopsis of Program. CDI programs are an integral component of effective revenue integrity initiatives under both fee-for-service and value-based payment.
Key words and phrases. CDI directors need stronger reporting and data analytics support. According to AHIMA Successful clinical documentation improvement CDI programs facilitate the accurate representation of a patients clinical status that translates into coded data.
When this happens the organization wins financially and earns higher quality rankings. Choose a CDI tool. This data must be highly accurate for medical advances including precision medicine artificial intelligence and advanced analytics capabilities to fulfill their promise of improving health outcomes.
Inpatient A common problematic situation is when CDI team members report to different levels of administration. Whether youre a veteran CDI specialist or new to the position or a physician advisor or HIMcoding professional youll want to take advantage of all the benefits of ACDIS membership including a career center CDI Journal CDI Forum sample forms and tools and much more. By implementing a CDI program they can help improve operational efficiency and ensure positive outcomes.
A CDI program in the outpatient setting can have just as much financial impact as in the inpatient setting. The survey also featured responses from staff in other healthcare settings that fell into the inclusion criteria for this survey 2102 percent showing CDI programs are branching beyond the traditional hospital arena. A CDI program is a virtual interactive cohort-based learning activity to help you build new skills and abilities.
It also creates unique opportunities to ensure that children are not denied benefits due to an institutions failure to meet Head Start andor CACFP requirements. Staffing is an issue. Data is the foundation for the future of healthcare operations.
The physicians documentation is utilized to populate the record with ICD-10 diagnoses. Lynne Spryszak RN CPC-A CCDS says in the article HIM CDI Programs Require TEAM Effort in JustCoding News. Monitor and Measure the CDI Program It is critical to closely monitor and manage the CDI Program along three primary drivers of success.
For physician practices clinical documentation is an important part of the patient encounter. In contrast a CDI virtual course is a self-paced virtual learning activity to help you generate new knowledge about a specific topic. Collaborative CDI requires a multidisciplinary team thats truly invested in clinical care improvement.
Computer-assisted-coding applications can be paired with _____________software technology to increase MCCCC capture rates. In both inpatient and outpatient CDI the physician is often simply an afterthought with the medical record serving as a reimbursement tool. If youve built your career on medical coding CDI may be an exciting new step in your professional development.
Provider offices rely on a healthy revenue cycle to ensure expenses and salaries are paid but claim denials or amendments because of improper code submission can be disruptive to the timely receipt of payment for services rendered. The concept search feature uses NLP to identify. ACDIS is the nations only association dedicated to the clinical documentation improvement profession.
Just like inpatient CDI programs outpatient CDI programs overlook first and foremost the physician in the mainstream of program design. Physician CDI Best Practices The primary focus of CDI for physicians in an office environment is to convey effectively through documentation a providers thought process regarding patient care. Compliance RatiosNet Revenue Impact Case Mix Index Volume Shifts by DRG SpecialtyMedical Surgical.
Hospitals should develop and establish CDI programs that focus on health information management and coding case management and continuity of care and quality reporting issues. The Future of Healthcare Depends on Effective CDI Programs. Typically two software modules are available to support the CDI program tasks including analytics and.
Poor documentation can impact code assignment reimbursement and. Cyber-Enabled Discovery and Innovation CDI is NSFs bold five-year initiative to create revolutionary science and engineering research outcomes made possible by innovations and advances in computational thinking. This document provides information on the basic principles and interventions recommended for the prevention of Clostridioides formerly known as Clostridium difficile infection CDI in acute care facilities.
HIM often reports to finance and the CDI specialists often report to case management who then reports. Computational thinking is defined. Consider exploring specialized audits and education for patient safety indicators hospital-acquired conditions risk adjustment for readmissions and 30-day mortality and risk adjustment for value-based payments.
Clinical documentation improvement CDI helps ensure EHR data is accurate for a variety of use cases such as quality reporting and patient care delivery. Collaboration lays the foundation for high-quality care that ultimately yields accurate reimbursement. Operational Quality and ComplianceFinancial Compliance Financial Performance Reports Metrics Measured.
Healthcare finance executives understand very well the positive impact of ensuring complete documentation to reflect the severity level of patients conditions drive quality outcome scores and support accurate payment for services.

Optimizing Clinical Documentation Improvement Huron

Core Indicators Of An Evaluation And Guidance System For Quality Of Care In Inflammatory Bowel Disease Centers A Critical Review Eclinicalmedicine
No comments for "Cdi Programs Are Best Applied in Which Situations"
Post a Comment